By Editor Spencer J Weinreich

Peter Bloodflower? (actually Samuel Palmer, Self Portrait [1825])
There are, however, those who dispute the existence of Bloodflower’s Melancholia in its hereditary form. Randolph Johnson is unequivocal on the subject. ‘There is no such thing as Bloodflower’s Melancholia,’ he writes in Confessions of a Disease Fiend. ‘All cases subsequent to the original are in dispute, and even where records are complete, there is no conclusive proof of heredity. If anything we have here a case of inherited suggestibility. In my view, these cannot be regarded as cases of Bloodflower’s Melancholia, but more properly as Bloodflower’s Melancholia by Proxy.’
If Johnson’s conclusions are correct, we must regard Peter Bloodflower as the sole true sufferer from this distressing condition, a lonely status that possesses its own melancholy aptness. (7)
One is reminded of the grim joke, “The doctor says to the patient, ‘Well, the good news is, we’re going to name a disease after you.’”
Master Bloodflower is not alone in being alone. The rarest disease known to medical science is ribose-5-phosphate isomerase deficiency, of which only one sufferer has ever been identified. Not much commoner is Fields’ Disease, a mysterious neuromuscular disease with only two observed cases, the Welsh twins Catherine and Kirstie Fields.
Less literally, Bloodflower’s Melancholia, RPI-deficiency, and Fields’ Disease find a curious conceptual parallel in contemporary medical science—or at least the marketing of contemporary medical science: personalized medicine and, increasingly, personalized diseases. Witness a recent commercial for a cancer center, in which the viewer is told, “we give you state-of-the-art treatment that’s very specific to your cancer.” “The radiation dose you receive is your dose, sculpted to the shape of your cancer.”
[youtube https://www.youtube.com/watch?v=DXeCLg0RiOM&w=560&h=315]
Put the phrase “treatment as unique as you are” into a search engine, and a host of providers and products appear, from rehab facilities to procedures for Benign Prostatic Hyperplasia, from fertility centers in Nevada to orthodontist practices in Florida.
The appeal of such advertisements is not difficult to understand. Capitalism thrives on the (mass-)production of uniqueness. The commodity becomes the means of fashioning a modern “self,” what the poet Kate Tempest describes as “The joy of being who we are / by virtue of the clothes we buy” (94). Think, too, of the “curated”—as though carefully and personally selected just for you—content online advertisers supply. It goes without saying that we want this in healthcare, to feel that the doctor is tailoring their questions, procedures, and prescriptions to our individual case.
And yet, though we can and should see the market mechanisms at work beneath “treatment as unique as you are,” the line encapsulates a very real medical-scientific phenomenon. In 1998, for example, Genentech and UCLA released Trastuzumab, an antibody extremely effective against (only) those breast cancers linked to the overproduction of the protein HER2 (roughly one-fifth of all cases). More ambitiously, biologist Ross Cagan proposes to use a massive population of genetically engineered fruit flies, keyed to the makeup of a patient’s tumor, to identify potential cocktails among thousands of drugs.
Personalized medicine does not depend on the wonders of twenty-first-century technology: it is as old as medicine itself. Ancient Greek physiology posited that the body was made up of four humors—blood, phlegm, yellow bile, and black bile—and that each person combined the four in a unique proportion. In consequence, treatment, be it medicine, diet, exercise, physical therapies, or surgery, had to be calibrated to the patient’s particular humoral makeup. Here, again, personalization is not an illusion: professionals were customizing care, using the best medical knowledge available.
Medicine is a human activity, and thus subject to the variability of human conditions and interactions. This may be uncontroversial: even when the diagnoses are identical, a doctor justifiably handles a forty-year-old patient differently from a ninety-year-old one. Even a mild infection may be lethal to an immunocompromised body. But there is also the long and shameful history of disparities in medical treatment among races, ethnicities, genders, and sexual identities—to say nothing of the “health gaps” between rich and poor societies and rich and poor patients. For years, AIDS was a “gay disease” or confined to communities of color, while cancer only slowly “crossed the color line” in the twentieth century, as a stubborn association with whiteness fell away. Women and minorities are chronically under-medicated for pain. If medication is inaccessible or unaffordable, a “curable” condition—from tuberculosis (nearly two million deaths per year) to bubonic plague (roughly 120 deaths per year)—is anything but.
Let us think with Bloodflower’s Melancholia, and with RPI-deficiency and Fields’ Disease. Or, let us take seriously the less-outré individualities that constitute modern medicine. What does that mean for our definition of disease? Are there (at least) as many pneumonias as there have ever been patients with pneumonia? The question need not detain medical practitioners too long—I suspect they have more pressing concerns. But for the historian, the literary scholar, and indeed the ordinary denizen of a world full to bursting with microbes, bodies, and symptoms, there is something to be gained in probing what we talk about when we talk about a “disease.”
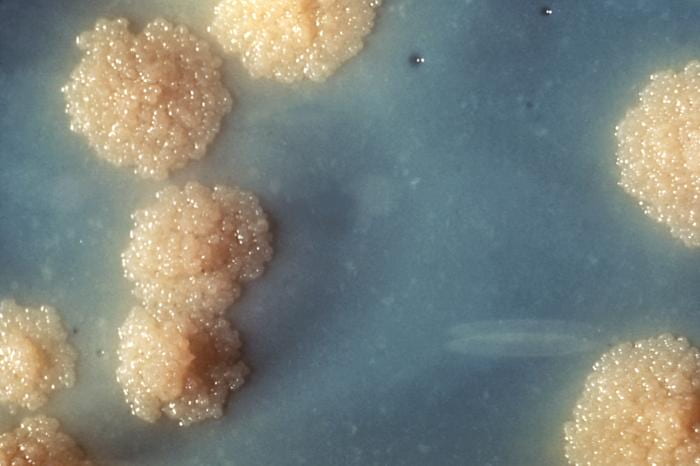
Colonies of M. tuberculosis
The question may be put spatially: where is disease? Properly schooled in the germ theory of disease, we instinctively look to the relevant pathogens—the bacterium Mycobacterium tuberculosis as the avatar of tuberculosis, the human immunodeficiency virus as that of AIDS. These microscopic agents often become actors in historical narratives. To take one eloquent example, Diarmaid MacCulloch writes, “It is still not certain whether the arrival of syphilis represented a sudden wanderlust in an ancient European spirochete […]” (95). The price of evoking this historical power is anachronism, given that sixteenth-century medicine knew nothing of spirochetes. The physician may conclude from the mummified remains of Ramses II that it was M. tuberculosis (discovered in 1882), and thus tuberculosis (clinically described in 1819), that killed the pharaoh, but it is difficult to know what to do with that statement. Bruno Latour calls it “an anachronism of the same caliber as if we had diagnosed his death as having been caused by a Marxist upheaval, or a machine gun, or a Wall Street crash” (248).
The other intuitive place to look for disease is the body of the patient. We see chicken pox in the red blisters that form on the skin; we feel the flu in fevers, aches, coughs, shakes. But here, too, analytical dangers lurk: many conditions are asymptomatic for long periods of time (cholera, HIV/AIDS), while others’ most prominent symptoms are only incidental to their primary effects (the characteristic skin tone of Yellow Fever is the result of the virus damaging the liver). Conversely, Hansen’s Disease (leprosy) can present in a “tuberculoid” form that does not cause the stereotypical dramatic transformations. Ultimately, diseases are defined through a constellation of possible symptoms, any number of which may or may not be present in a given case. As Susan Sontag writes, “no one has everything that AIDS could be” (106); in a more whimsical vein, no two people with chicken pox will have the same pattern of blisters. And so we return to the individuality of disease. So is disease no more than a cultural construction, a convenient umbrella-term for the countless micro-conditions that show sufficient similarities to warrant amalgamation? Possibly. But the fact that no patient has “everything that AIDS could be” does not vitiate the importance of describing these possibilities, nor their value in defining “AIDS.”
This is not to deny medical realities: DNA analysis demonstrates, for example, that the Mycobacterium leprae preserved in a medieval skeleton found in the Orkney Islands is genetically identical to modern specimens of the pathogen (Taylor et al.). But these mental constructs are not so far from how most of us deal with most diseases, most of the time. Like “plague,” at once a biological phenomenon and a cultural product (a rhetoric, a trope, a perception), so for most of us Ebola or SARS remain caricatures of diseases, terrifying specters whose clinical realities are hazy and remote. More quotidian conditions—influenza, chicken pox, athlete’s foot—present as individual cases, whether our own or those around us, analogized to the generic condition by memory and common knowledge (and, nowadays, internet searches).
Perhaps what Bloodflower’s Melancholia—or, if you prefer, Bloodflower’s Melancholia by Proxy—offers is an uneasy middle ground between the scientific, the cultural, and the conceptual. Between the nebulous idea of “plague,” the social problem of a plague, and the biological entity. Yersinia pestis is the individual person and the individual body, possibly infected with the pathogen, possibly to be identified with other sick bodies around her, but, first and last, a unique entity.

Newark Bay, South Ronaldsay
Consider the aforementioned skeleton of a teenage male, found when erosion revealed a Norse Christian cemetery at Newark Bay on South Ronaldsay (one of the Orkney Islands). Radiocarbon dating can place the burial somewhere between 1218 and 1370, and DNA analysis demonstrates the presence of M. leprae. The team that found this genetic signature was primarily concerned with the scientific techniques used, the hypothetical evolution of the bacterium over time, and the burial practices associated with leprosy.
But this particular body produces its particular knowledge. To judge from the remains, “the disease is of long standing and must have been contracted in early childhood” (Taylor et al., 1136). The skeleton, especially the skull, indicates the damage done in a medical sense (“The bone has been destroyed…”), but also in the changes wrought to his appearance (“the profile has been greatly reduced”). A sizable lesion has penetrated through the hard palate all the way into the nasal cavity, possibly affecting breathing, speaking, and eating. This would also have been an omnipresent reminder of his illness, as would the several teeth he had probably lost (1135).
What if we went further? How might the relatively temperate, wet climate of the Orkneys have impacted this young man’s condition? What treatments were available for leprosy in the remote maritime communities of the medieval North Sea—and how would they interact with the symptoms caused by M. leprae? Social and cultural history could offer a sense of how these communities viewed leprosy; clinical understandings of Hansen’s Disease some idea of his physical sensations (pain—of what kind and duration? numbness? fatigue?). A forensic artist, with the assistance of contemporary symptomatology, might even conjure a semblance of the face and body our subject presented to the world. Of course, much of this would be conjecture, speculation, imagination—risks, in other words, but risks perhaps worth taking to restore a few tentative glimpses of the unique world of this young man, who, no less than Peter Bloodflower, was sick with an illness all his own.

1 Pingback