By John DiMoia

With South Korean elections held in mid-April (April 15th), one of the major issues became the Moon Jae-in government’s handling of the COVID-19 crisis. Though briefly one of the world’s leading countries in terms of the number of cases as of mid-February, the nation has since earned international praise for its ability to “flatten the curve,” quickly reducing the number of cases through an intensive testing and tracing program. Indeed, the government has been quick to claim credit for the collective response of its public health workers, earning public trust, and aiming for electoral success. Still, the question remains: which experiences in the Korean past contributed to this impressive output? Could it be, as some have suggested, that the experience of SARS played a role?
Following the SARS (Severe Acute Respiratory Syndrome) outbreak of 2003, governments throughout the greater East and Southeast Asian region mobilized the lessons they claim to have “learned from SARS.” This was certainly the case with H1N1 (2009) in Singapore; and later, with the MERS (Middle East Respiratory Syndrome) outbreak which took place in South Korea (2015). Although the analogy to SARS is understandable, an easily available comparison, I suggest here that there are much richer possibilities in the Korean past for understanding the present circumstances of COVID-19. Although SARS is clearly an important precedent, the disease carries with it a great deal of ideological baggage, seeking to blame China specifically for a failure to ensure reliable reporting of cases, and for a corresponding failure to be transparent and maintain communication with international institutions. It was MERS, rather than SARS, which helped to reshape the South Korean experience, especially as it surprised a large number of people, including those in charge of the public health system.
Public Health: Origins in Successive Crises
Before touching on MERS, we should first recall the spread of epidemic disease in the late 1940s as the formative context for public health in Northeast Asia, especially following the closing weeks of World War Two. Japan neglected the peninsula’s infrastructure in the later war years, given the need to fight on multiple fronts. In 1945 and following, with the Korean War (1950-1953) soon to come, the migration of refugees between China, Japan, and South Korea led to frequent outbreaks of cholera and typhus. The joint occupations of Japan (1945-1952) and South Korea (1945-1948), along with the resumption of China’s civil conflict (1945-1949), heightened concerns for American military authorities. During the Korean War, the hanta virus, manifesting itself in the form of hemorrhagic fever, led to kidney ailments for combatants regardless of their ideology, and some historians have speculated about linking this development to Chinese and North Korean allegations of biological warfare. As a coda to this story, Dr Ho Wang Lee, a Korean physician, isolated the virus in 1976, bringing a successful result to a quest beginning with the war.
If the rapid spread of epidemic disease in the region lingers powerfully in Korean memory, a related point concerns the South Korean public health system as an ongoing set of bureaucratic institutions, a significant number of which derive their origins in part from late Japanese colonial rule (1910-1945) and the subsequent period of Korean military rule (1961-1987). The period spanning the late 1940s through the 1970s witnessed the gradual introduction of national health insurance (1963, 1977), with major reforms coinciding with the arrival of democratization (1989). At about the same time (1954-1960) as the earliest forms of health insurance, many South Korean hospitals received international aid in the aftermath of the Korean War, and began transforming their approach to clinical practice with new resources and medical pedagogy from Europe (Norway, Sweden, and Denmark) and the United States (University of Minnesota). If South Korea now possesses biomedical facilities more than capable of handling any crisis, the practices and institutional norms at these sites were nonetheless acquired under very different conditions at mid-20th century. This was medical care directed at an emergency situation, one filled with refugees, bodies, and the exigencies associated with wartime conditions and its immediate aftermath.
With these difficult circumstances, beginning in the late 1950s, South Korea pursued a series of ambitious national health campaigns, first targeting chronic disease, such as leprosy, tuberculosis, and malaria, often working in conjunction with the WHO (World Health Organization). These campaigns were followed by additional schemes, associated with a heavy dose of social engineering, here including Family Planning (1964-mid 1980s), and Anti-Parasite Campaigns (1968-early 1990s). Once again, efforts were carefully coordinated with international partners and institutions, including the Population Council and Japanese technical cooperation (JICA, Japan International Cooperation Agency). Moreover, the second of these campaign, targeting parasites, focused on school-age children, requiring them to submit stool samples on a bi-annual basis, with teachers collecting the “data” before it was analyzed. The stories from these campaigns indicate that there was a good deal of unfamiliarity with the Korean state’s goals, and sometimes, embarrassed students avoided school, or submitted a pet’s sample in place of their own. Only through concerted efforts, including posters, print ads, and public outreach could the government make its public health intentions clear. The generations of Koreans raised in the post-Korean War era through the early 1980s soon learned to become familiar with frequent health interventions (inspections, vaccinations, samples), whether at school, the office, or comparable public institutions.
The MERS Mishap (May-June 2015)
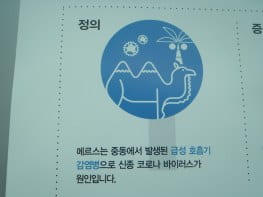
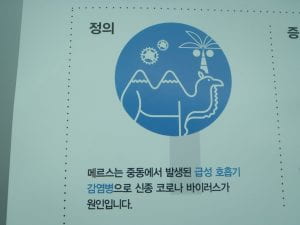
Give this successful legacy of national campaigns, and a developmental trajectory often assumed to be “progressive,” the MERS scenario began modestly, with health authorities assuming that it would not represent a major problem. The disease was framed as a “foreign” problem, with MERS manifesting itself in 2012, and only three years later appearing in Korea. Posters placed at Incheon airport, and also at rail and bus stations, typically depicted a camel and a palm tree (see Figure One) to underscore the external nature of the virus, which would require a Korean to travel through the region to be exposed. One famous poster illustrated the disease with a bactrian, or two-humped camel (see Figure Two), which is not the species associated with the spread of MERS. A relaxed attitude, and the freedom of movement permitted to possible cases, caught the system by surprise, leading to a genuine health problem, and a related political problem for the government of President Park Geun-hye. This series of events soon became the largest outbreak of MERS to occur outside its original setting.
The diverse stories emerging during the spread of MERS illustrate a strong continuity with earlier historical developments, as the first patient traveled to four hospitals over a nine-day period, seeking a diagnosis, with uncertain symptoms. In the course of this movement, this individual, along with others to follow, some of whom broke quarantine, infected surrounding individuals, and also the surrounding space of health care facilities. In turn, after the outbreak became public knowledge, Korean patients sought to gain access to major health facilities in Seoul, often with crowded, inhospitable conditions in the wards. The structural inequities of the nation’s health care system—the rural / urban divide, geographical isolation, access to public health care in a system strongly favoring its more lucrative, private side—are certainly not new, and very likely exacerbated conditions as MERS made its way rapidly through hospitals, ultimately killing thirty-eight individuals, out of one hundred eighty-five confirmed cases. The largest MERS outbreak to take place outside of the Middle East, this incident served as a critical wake-up call.
As South Korea grapples with COVID-19, receiving a great deal of praise for its series of rapid testing, drive-in checkpoints, contact tracing, and the distribution of masks, we should remember that these developments cannot be attributed to culture, a set of attitudes, or be credited to a narrow set of political interests. If it is reasonable to screen for elevated temperature and related symptoms, we also need to be careful about assuming ready consent upon the part of all Koreans, and to recognize that much of the domestic criticism of the Moon Jae-in government does not make the international press. In fact, the link of the virus to the Shincheonji church has been controversial, with some elderly Koreans complaining about their treatment, and the disruption of church services (see Figure Three).
Ultimately, the MERS outbreak in the region, tied to a longstanding legacy of institutional and structural inequities, brought much-needed attention to these kinds of issues within the Korean health system. A bureaucracy with a lengthy history, health care in South Korea derives from the period of transition following colonialism and two wars—Korean participation in Vietnam (1964-1973) was also extensive, and featured the nation’s first overseas medical outreach—and it holds onto a deeply ingrained set of practices, many of which require periodic updating. MERS became the critical factor calling attention to this need, and the renewed practices of 2020 started only in the intervening period, especially the use of rapid and effective testing.
Coda: This analysis was written prior to the ROK elections held on April 15,,2020. The ruling party of President Moon went on to win an electoral majority. The ROK government has since issued its version of the COVID-19 story as a pamphlet, and it can be found here:
How Korea responded to a pandemic using ICT: Flattening the curve on COVID-19
Suggested Readings:
- Nicole Barnes, Intimate Communities: Wartime Healthcare and the Birth of Modern China, 1937-1945 (University of California Press)
- Mary Brazelton, Mass Vaccination: Citizens’ Bodies and State Power in Modern China (Cornell University Press)
- A Homei and J DiMoia, “Integrating Parasite Eradication with Family Planning: The Colonial Legacy in Post-war Medical Cooperation in East Asia” (forthcoming, Social History of Medicine)
- Jeong-ran Kim, “The borderline of ’empire’: Japanese maritime quarantine in Busan c.1876-1910,” Medical History. 2013 Apr;57(2):226-48
- Kyuri Kim, Buhm-soon Park, “Infrastructure-building for Public Health : The World Health Organization and Tuberculosis Control in South Korea, 1945-1963,” Korean Journal of Medical History 2019; 28(1): 89-138.
- Sonja Kim, Imperatives of Care: Women and Medicine in Colonial Korea (Hawai‘i Studies on Korea) (University of Hawaii Press)
- Mark Harrison and Sung Vin Yim, “War on Two Fronts: The Fight against Parasites in Korea and Vietnam,” Medical History, Volume 61, Issue 3 July 2017 , pp. 401-423
- Youngsu Park, Tempoethics: Envisioning Asian Modernities and Enacting Global Health Projects in Ethiopia (Ph.D. dissertation, Anthropology, Stanford University)
- Wayne Soon, Global Medicine in China: A Diasporic History (Stanford University Press, forthcoming)
- Joseph Wong, Healthy Democracies: Welfare Politics in Taiwan and South Korea (Cornell University Press)
John DiMoia is Associate Professor in the Department of Korean History at Seoul National University. He is the author of Reconstructing Bodies: Biomedicine, Health, and Nation-Building in South Korea since 1945 (Stanford University Press / WEAI 2013), and with Hiromi Mizuno and Aaron S Moore, one of the co-editors of Engineering Asia: Technology, Colonial Development and the Cold War Order (Bloomsbury / WEAI 2018).


May 23, 2020 at 9:37 am
Thanks for your work. This is really a very interesting and relevant article for today!