by Khushboo Rashid
Much like medieval Europe, the South Asian subcontinent was exposed to the ravages of the plague at several turns. Recent scholarship has focused on the historical details of various episodes of the plague that affected South Asia during the early modern period, yet the task of elucidating the doctrine that dictated physicians’ and states’ responses to contagion has been overlooked. The following discussion endeavors to demonstrate how court physicians in Mughal India employed the notion of contagion and implemented prophylactic measures accordingly to cope with the catastrophic consequences of the plague.
The plague was one of the many lethal diseases in Mughal India that kept occurring in seasonal patterns. It decimated Mughal India’s population, in addition to the heavy toll caused by famine. The frequent plague outbreaks in South Asia posed a serious challenge to medical practitioners of Yūnānī ṭibb (Greco-Arabic medicine) regarding their knowledge, procedures, and measures. Physicians found themselves saddled with the unenviable responsibility of explaining why an almost inconceivable number of people of different ages and sexes were dying from rapidly spreading and mysterious diseases. The emergence of pestilential diseases (including syphilis and smallpox) questioned the traditional humoral framework of ṭibb for the causation of ailment, as they did not adhere to its fundamental principle. The humoral theory posits that a disease results from the imbalance of four humors—blood, phlegm, black bile, and yellow bile present within the body. According to this theory, each individual possesses a unique humoral equilibrium, leading to variations in the manifestation of illnesses. The populace suffering from the same disease not only raised serious questions about the validity of the humoral theory but also highlighted the need for a new approach to understanding the causes of some of the new contagions.
In the popular opinion, a range of external factors, such as divine punishment, spiritual, astrological, meteorological, and environmental, were blamed for the causation of epidemics. However, Mughal physicians favored the miasmatic vapor or poisonous air in the environment as the primary and decisive causative factor for infectious diseases, as the air was the only common factor physicians could identify as being shared by the sick. This notion was considered adequate to explain the simultaneous appearance of similar symptoms and signs among individuals. As a result, a new medical paradigm of putrid or foul air (ufūnat-i hawa) emerged in medical literature, signifying a momentous shift in medical thinking of Mughal South Asia.
In medieval Greco-Arabic medical literature, the concept of miasma was critical in identifying specific diseases based on their transmissible nature. The air of the surroundings was an essential factor for a healthy body in the ṭibb. The toxic air (fasād-i hawa) inhaled from the surrounding areas was believed to be detrimental to the functioning of the body’s vital organs (aʿżā-ī raīsah), mainly the mind and brain. According to the prominent physicians of Greco-Arabic medicine, Jalius (Galen, d. 216) and Ibn Sīnā (Avicenna, d. 1037), inhaled air exerted an influence on the faculty of smell (ḳuvāt- ī s̲h̲āma) placed in the brain and affects the ability of the heart to pump the humors to the whole body, resulting in hindered functioning of the brain and heart. A foul or fetid setting was believed to be inimical to the physiological processes of the body. The entry of unpleasant air into the body hindered the functioning of vital organs, impeding the brain’s ability to master intelligence, the stomach’s capacity to produce humors in balanced quantities, and the heart’s strength in circulating humors throughout the body. Mughal emperor Jahangir (d. 1627) drew on his personal experience, mentioned in his autobiography Tuzuk-ī Jahāngīrī, that people who inhaled bad air (bad-bū) were incredibly weak-hearted, feeble-minded, wretched, and suffered from various ailments. Fresh and fragrant air, on the contrary, was perceived as a fortified entity against these virulent diseases.
The earliest Persian medical text in South Asia discussing the correlation between a polluted atmosphere and epidemic diseases (emrāż-ī wabā), notably plague, was Ilājāt-i Dārā Shikohi composed by Mughal physician Nur-ud Din Muhammad Abdullah Shirāzī (d.1650).It is a voluminous medical work dedicated to Mughal prince Dara Shikoh. (d. 1659) In Ilājāt-i Dārā, Hakim Shirazi gave a detailed account of the signs, symptoms, and etiology of the plague (ṭāʿūn), considering it one of the deadliest diseases of the time. He wrote that “plague is caused by contact with the foul air (fasād-ī hawa), which further corrupts the blood (dam). The toxic substance (mādah-i Sammīyat) impeded the functioning of vital organs of the body, such as the heart and its surrounding organs. The poisonous substances of the plague reach the heart through the arteries and cause vomiting and suffocation.” Hakim Shirazi also noticed that the color of the body changed to black when ṭāʿūn reached its last stage. The symptoms of the plaguedescribed by all medieval medical authorities were similar. Hakim Shirazi stated that ṭāʿūn causes severe fever, headache, unconsciousness, and purulent swellings (dāna) of the walnut size that appear on lymph nodes of the body such as under the armpits, on the chest, groins, behind the ears or below the throat. Notably, the Mughal emperor Jahangir, in his memoir,described identical symptoms, suggesting the population of Mughal India was suffering from bubonic plague, one of the threatening diseases of the early modern period, also commonly known as black death. Hakim Shirazi also provided Hindavi terminology for ṭāʿūn (dar hindi gūyund) as Laut, Behravi, and Bebonje. The practice of incorporating the vernacular names of ailments and medicine was an essential feature of South Asian medicines, witnessing ongoing interactions between authoritative physicians and local healers.
Ilājāt-i Dārā displays a growing recognition of the role of proximity in the spread of epidemic diseases, marking a significant shift in medical thinking in Mughal India. In the section on plague, Hakim Shirazi strongly advised isolating the infected from healthy individuals as the plague was mutaʿaddī (contagious). The term mutaʻaddī was commonly used by Persian medieval physicians to differentiate certain diseases based on their nature of transmissibility. It encompassed the notion of touch, transmission, transitiveness, and the passage of something from one locus to another. Metaphorically, this term was used to elicit the fear of proximity with the sick, as they were considered an agent of defilement. In such cases, the English translation “contagion” of mutaʻaddī seems quite appropriate. However, the term contagion carries a modern epidemiological definition of disease transmission through micro-organisms, which is seldom limited here. The term mutaʻaddī is employed to elucidate the pre-modern concept of transmission of diseases through putrid or corrupted air.
In Mughal South Asia, the general relation between atmospheric phenomena and epidemic diseases was not confined to the intellectual elites. Instead, it was widely acknowledged and accepted by a significant portion of the Mughal population. For instance, in his memoir, Mughal emperor Jahangir gave a gloomy description of Gujarat’s weather during his visit. He recalled that due to the excessive heat and corruption of the air, most of the city’s people and imperial camp members, including him, fell severely sick from an attack of inflammatory fever. In the account of the Assam expedition during the reign of Mughal emperor Aurangzeb (d.1707), court historian Saqi Mustad Khan blamed the outbreak of pestilences in Assam on poisonous air produced after continuous rain. The plague affected the whole land of Assam and carried off vast numbers of inhabitants. Thus, the miasmatic theory played a central role both in identifying the source of diseases and hindering the physiological processes of the body.
As a result of these experiences and inventions, public health and hygiene notions in the Mughal period centered around the problem of “corrupted and poisoned air.” Yūnānī ṭibb tradition accentuated atmospheric air (hawa-i muhit) as the foremost factor for disease causation. Thus, maintaining the correct air balance became the principal concern of early modern physicians. Mughal medical treatises repeatedly emphasized the necessity of avoiding foul-smelling places like graves, swamps, or narrow streets, where evil vapors could not dissipate properly.
Importantly, even the Mughal state related dirt to diseases and reiterated the need for the disposal of dirt from residential areas. Consequently, the Mughal state adopted essential measures to improve public hygiene. For instance, Mughal emperor Akbar (d. 1605) assigned kotwals in each province to relocate polluted and foul-smelling regions such as slaughterhouses, tanneries, dead body washing houses, execution houses, and cemeteries outside the residential areas. Kotwals were also entrusted with the task of cleaning and maintaining the public streets free from garbage and foul smells. These measures were employed to halt the spread of noxious air in urban and rural areas and intended to reduce the likelihood of plague outbreaks.
During epidemic outbreaks, court physicians reassured the public that the plague could be cured and provided practical advice during plague outbreaks. Two principal methods were advised to protect from toxic air: filtering the smell using various aromatic substances and abandoning disease-stricken regions. Mughal physicians recommended aromatic preventive measures to protect against the disease by neutralizing its smell. They included several medical-olfactory prescriptions in their medical texts to ward off the poisonous air and improve air quality within homes and their surroundings. Persian medical treatises are full of recipes for making fragrances, aromatic oils, and syrups that would keep the stench of air away. In Yūnānī Ṭibb’s setting, odoriferous substances were considered the chief fortifiers of vital organs- heart and brain from noxious air. These ingredients exhilarate the heart by reviving the “vital spirit” of the body (also called rūh), thereby ensuring the proper functioning of the body.
The famous court physician of the Mughal emperor Aurangzeb, Hakim Akbar Arzāni (d.1722), outlined specific precautions to follow during plague outbreaks in his medical text Mīzān-ī Tibb. He recommended the purification of oneself and the surrounding area, which he called taniqat-wa- taṣfiya (to purify). Following the plague outbreak, Arzāni advised cleaning the entire body, house, and windows using perfumed water made of medicinal herbs such as willow leaves, lotus flowers, violet plants, roses, camphor, and sandalwood. He suggested fumigating the whole house every hour with the mixture of vinegar and rose water, as physicians held this mixture to protect from foul air efficiently. Indoors, houses were to be infused with medical-olfactory aromatic incense called lakhlakha, composed of aloeswood, musk, and camphor, which physicians recommended to burn in-house to drown the stench under wafts of their perfumes. Additionally, he emphasized the importance of cleaning oneself and one’s house, as maintaining cleanliness outside was more challenging. Physicians warned people not to go outside during the epidemic and not to let external air enter their home confinements.
Mughal physicians emphasized the importance of both internal and external exhalation of good scents. They promoted medical-olfactory prescriptions to fortify vital organs from the toxic air entering the body. The fragrant and aromatic medicinal commodities were considered a fortifier and chief nourishment of the heart (ghizah-i ruh). The famous 11th-century physician Ibn Sīnā, in his treatise Al-adwiyyā al-qalbiyyā (The Medicine of Heart), discussed the relation of aromatic drugs with heart health as the protector of the heart. In a similar vein, Mughal physician Hakim Shirazi, in his Ilājāt-i Dārā, prescribed frequent intakes of cardiac tonic (maqawi-i dil), such sherbat (juice) of apple, sandalwood, lemon, orange, rose, pomegranate, and sour soup of tomatoes to strengthen and protect the heart during the epidemic.
Mughal medical literature offers invaluable insights into how medical practitioners and public authorities mitigated plague outbreaks in early modern South Asia. The writings of Mughal physicians highlight the central role of the concept of miasma, or a polluted environment, in understanding the idea of contagious disease, a notion that was at the time unanimously accepted by all segments of society. The origins of this concept can be traced back to the earlier contributions made by renowned physicians such as Galen and Ibn Sīnā, who influenced the miasmatic framework. Simultaneously, an important paradigm shift in medical thinking occurred with the emergence of the concept of person-to-person disease transmission during the early modern resurgence of epidemics. As a result, Mughal medical practitioners pioneered innovative prophylactic measures, including indoor fumigation, restricted movement, the use of aromatics, and house arrest, which gained support from the local authorities to mitigate the spread of disease.
Because of its Eurocentric bias, much of the historiography about medicine and science has long marginalized the scientific advancements in health and hygiene in other parts of the globe. The observations offered in this article falsify orientalist assumptions about public health systems in pre-colonial South Asia. Rather, the analysis of Persian sources reveals that Mughal physicians, grounded in empirical observations of mortality and morbidity, promoted a sophisticated and innovative comprehension of hygiene. Consequently, this notion of contagion played a pivotal role in shaping Mughal state policies about public health to limit the impact of the plague.
Khushboo Rashid, currently a PhD candidate in the Department of History and Culture at Jamia Millia Islamia, India, is a Fulbright Scholar at the University of Washington, Seattle. Her dissertation, entitled “Medicine, State, and Society: The Role of Physicians in Mughal India, ca. 1526-1707,” uses a transregional approach to examine the circulation and exchange of medical knowledge (Yūnānī ṭibb), practices, medical commodities, and scientific illustrations during the formative era of global connectivity. Her focus is on providing decolonised perspectives on medical knowledge and practices in early modern South Asia by analysing a wide range of sources, including Persian medical treatises, courtly chronicles, and European travelogues. Her research has received significant support from the Indian Council of Historical Research.
Edited by Nilab Saeedi
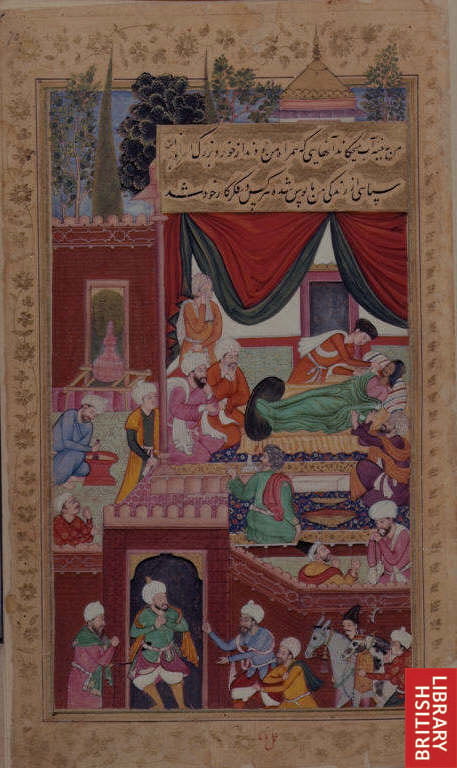
Featured Image: Babur being treated by physicians, an illustration from Baburnama (a memoir of Mughal Emperor Babur), painted by Nanha. British Library, Public Domain, Via Wikipedia Commons.